The last Monday, the World Tuberculosis Day was celebrated with the aim of raising awareness about the need to raise more funds to address it. These are some of the most common questions about this disease.
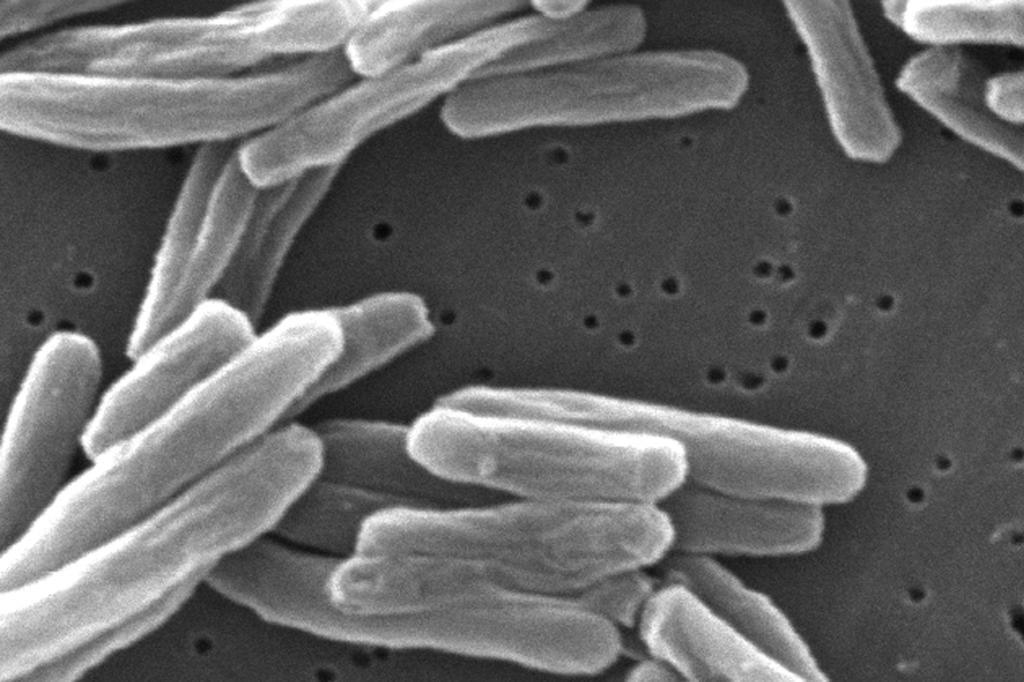
Tuberculosis is a disease caused by Mycobacterium tuberculosis (Koch), a bacterium that usually affects the lungs. It is curable if the appropriate treatment is administered and can be prevented.
The infection is transmitted from person to person through the air. When a person with pulmonary tuberculosis coughs, sneezes, or spits, they expel tuberculous bacilli into the air. Inhaling a few bacilli is enough to become infected. However, not all infected individuals develop the disease. It is estimated that one-third of the world's population has latent tuberculosis, although only 10% are at real risk of becoming ill.
The most common symptoms of tuberculosis are cough (sometimes with blood in sputum), fever, night sweats, weight loss, and chest pain. However, symptoms can present mildly for months, and patients often take a long time to seek medical attention, posing an added risk of disease spread.
Which groups are at higher risk of infection?
Tuberculosis has a special incidence in young adults, although all age groups are at risk. Over 95% of cases and deaths occur in developing countries. Individuals infected with HIV and the tubercle bacillus are 21 to 34 times more likely to become ill. Children are also particularly vulnerable. In 2011, half a million new cases were detected in children aged 0 to 14, and around 64,000 died from this cause.
What is the incidence of tuberculosis worldwide?
According to the WHO, in 2023, 10.8 million cases of the bacterial disease were diagnosed worldwide, compared to 10.7 million in 2022. The upward trend is global and is also reflected in Spain, which, according to data from the Spanish Society of Epidemiology (SEE), after experiencing a decline between 2015 and 2019, resurged after the pandemic. In 2023, cases increased by 11.4% compared to 2021, with a notification rate of 8.2 cases per 100,000 inhabitants, although there are differences among autonomous communities.
The regions with the highest rate of cases were Catalonia (12.3), Galicia (11.2), and the Basque Country (10.9) according to data from the National Epidemiological Surveillance Network and the Plan for the Prevention and Control of Tuberculosis in Spain.
Tuberculin (PPD) or Mantoux test: involves injecting an extract containing antigens of the Koch bacillus into the subcutaneous tissue, which cannot cause infection since it does not contain the entire bacillus.
If a person has antibodies against the bacillus, they will have a cutaneous reaction 2-3 days after inoculation, characterized by induration, erythema, and warmth. If this reaction occurs, it means that the individual has been in contact with the bacillus at some point in their life.
This does not mean that there is an infection at the time of the test, but if the clinical circumstances are appropriate, it can help establish the diagnosis.
A definitive diagnosis is made by isolating and identifying the bacillus in culture media.
The Koch bacillus has a great ability to protect itself against antibiotics by developing resistance when these are used individually. Therefore, the use of antibiotic combinations is always necessary.
Treatment can be done on an outpatient basis, although respiratory isolation is required, at least for the first two weeks.
Among the first-line antitubercular drugs are isoniazid, rifampicin, pyrazinamide, ethambutol, and streptomycin.
International infectious disease associations currently recommend starting treatment with three first-line antibiotics for two months, followed by two of them for an additional four months.
The most common treatment regimen is a combination of isoniazid, rifampicin, and pyrazinamide for the first two months, followed by isoniazid and rifampicin for another four months. Depending on the cases, longer and more drug-intensive regimens may be necessary.
With the treatments available today, the prognosis for tuberculosis is excellent.
Generally, two weeks after starting treatment, the infected patient stops being contagious, and a progressive recovery of the general condition begins. Within a few weeks, most patients can lead a normal life and return to work, according to the University Clinic of Navarre.