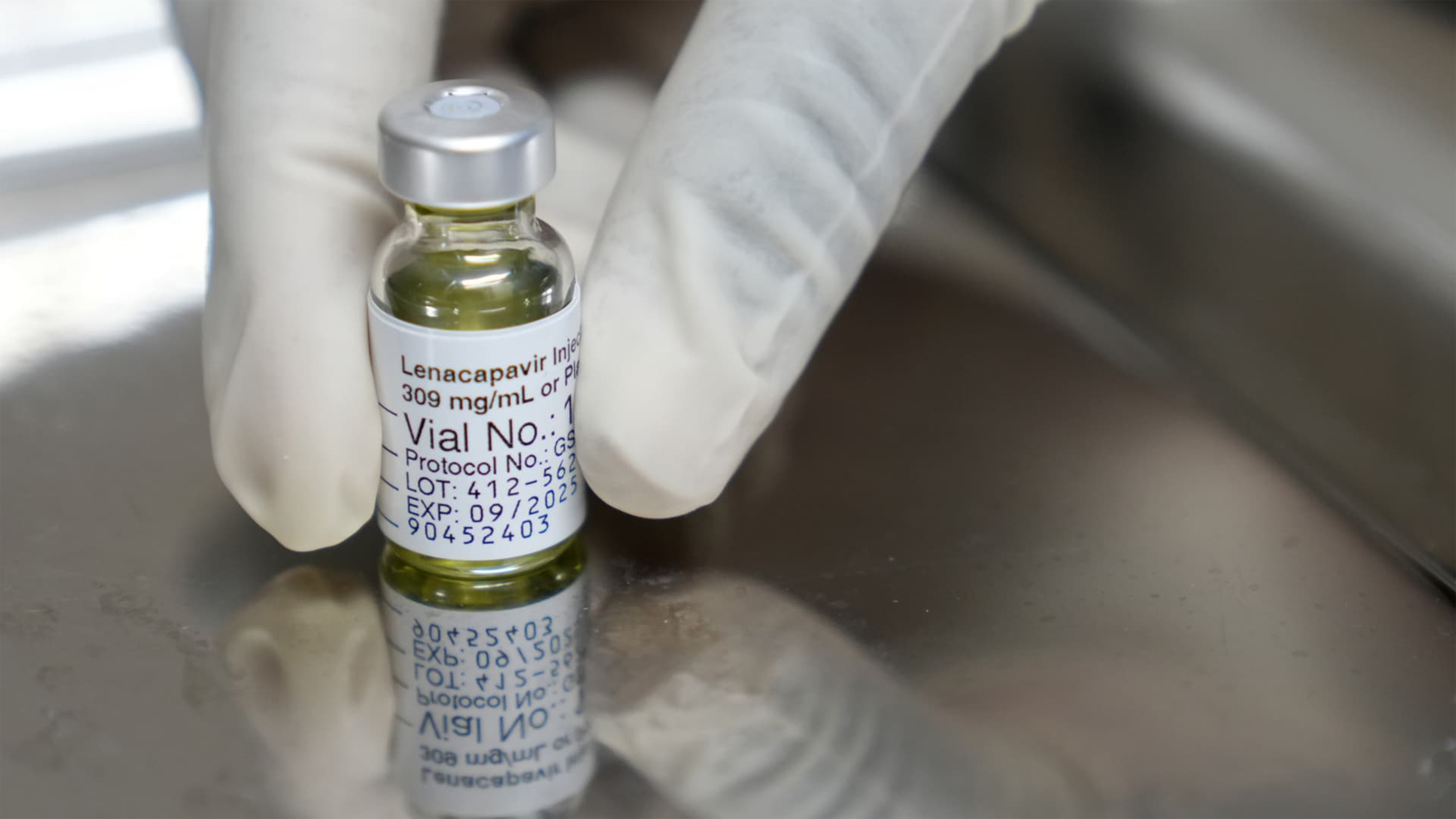
From two injections per year to one against HIV. "It is a hopeful step and the study data are positive." María Velasco, spokesperson for the Spanish Society of Infectious Diseases and Clinical Microbiology (Seimc), values the results of a phase 1 trial on the use of intramuscular injection of lenacapavir to create a shield against the infection.
This study that evaluates an annual injection of a pre-exposure prophylaxis medication for HIV has been published in The Lancet and presented simultaneously at the Conference on Retroviruses and Opportunistic Infections (CROI). The trial demonstrates that medication concentrations remain in the body for at least 56 weeks.
The semi-annual version is under review by regulatory agencies in Europe for approval. Meanwhile, its counterpart in the US, the FDA, could use the fast track or accelerated review for this purpose. The potential of the drug, developed by Gilead, to contain the spread of infections used in at-risk individuals as pre-exposure prophylaxis, known as PrEP, earned it recognition as the discovery of the previous year by Science magazine.
PrEP is a type of medication used to prevent HIV infection in individuals at risk of exposure to the virus, preventing its entry and replication in human cells. Currently, it is approved in the form of a daily pill. When taken correctly, PrEP has an efficacy of over 90% in preventing HIV. The semi-annual injection reaches almost 100%
However, in 2023, only 3.5 million out of the 21.2 million people who would benefit from PrEP were receiving it, highlighting the need to eliminate existing barriers, such as stigma and discrimination, limited access to health clinics, lack of adherence to currently available regimens, and the cost of medication, even through longer-acting PrEP options.
Velasco makes it clear that neither this annual injection nor PrEP pills are the same as vaccines, and currently, there is no vaccine available to prevent HIV. "However, these types of long-acting medications are very useful in population groups where oral forms [pills] do not quite work, such as in women." For the Gesida spokesperson, "we are on the brink of a new era in HIV."
What has the new trial shown?
In the new study, 40 HIV-negative participants aged between 18 and 55 years were injected with one of the two lenacapavir formulations administered as a single dose. Samples were collected at pre-specified time points up to 56 weeks to evaluate the safety and pharmacokinetics (how a drug moves through the human body) of the injection.
Overall, the medication was well tolerated, with injection site pain being the most common adverse event. "We will have to see if it behaves the same way in phase two, especially in terms of tolerability," says Velasco, also the secretary of the Gesida group. The study also notes that no clinically significant safety issues were identified.
After 56 weeks, the average plasma concentrations of intramuscular lenacapavir exceeded those associated with efficacy in phase 3 studies of a subcutaneous injection (an injection under the skin and above the muscle tissue) of the injectable twice a year for PrEP. "We see how in the study the results are compared with Purpose 1 and 2 trials, which were conducted to measure its semi-annual action," points out Velasco.
As this was a phase 1 study, its purpose was to measure safety and the body's physiological response. Therefore, there is still no data to ensure efficacy in preventing HIV infection, and more clinical trials are needed, "even with participants from more diverse population groups," Velasco argues about the challenges that phase 2 trials will face.
"They must include an explicit diversity of volunteers by race, gender, and social conditions to be able to extrapolate the data," notes the Gesida spokesperson. These studies will already involve a sample size exceeding one hundred individuals.
The authors state that expanding PrEP options, such as a possible annual injection, can help overcome current barriers to access and adherence and drive progress towards reducing new HIV infections.